Mixing Benadryl and alcohol is a common but dangerous practice that many people underestimate.
Combining these two central nervous system depressants produces synergistic impairment, meaning the combined effect is greater than either substance alone, significantly increasing your risk of drowsiness, falls, impaired driving, and serious cognitive deficits.
This article explains what happens when you mix Benadryl and alcohol, who is most at risk, and what safer alternatives exist.
What Happens When You Mix Benadryl and Alcohol?
When you combine diphenhydramine (the active ingredient in Benadryl) with alcohol, you create a dangerous synergy.
Diphenhydramine is a first-generation antihistamine that readily crosses into your brain, where it blocks histamine receptors and muscarinic receptors, producing sedation and anticholinergic effects.
Alcohol acts as a CNS depressant through different mechanisms, impairing attention, reaction time, and motor coordination. Together, they amplify each other’s effects in ways that can be unpredictable and severe.
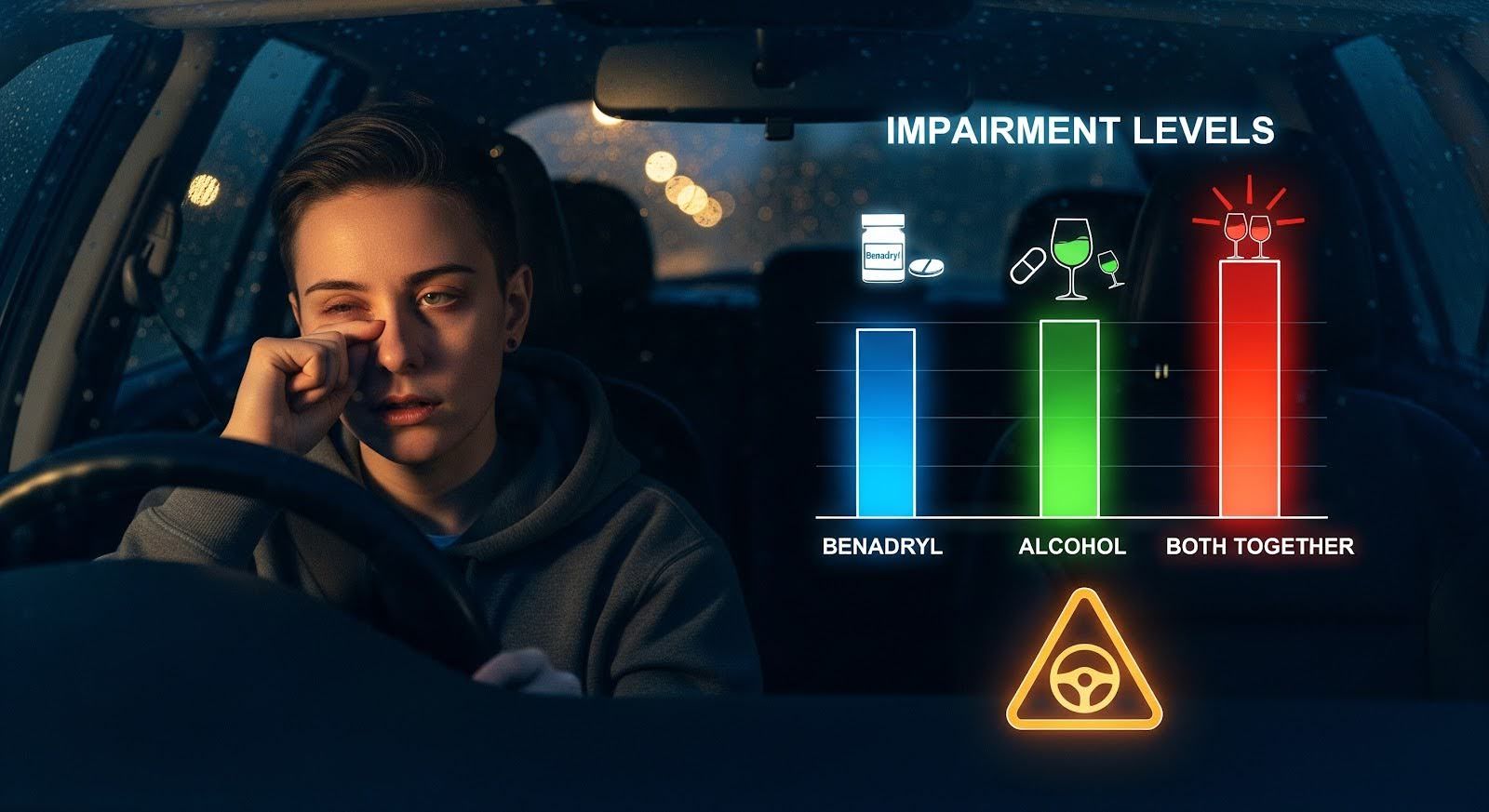
Research using high-fidelity driving simulators demonstrates that a single 50 mg dose of diphenhydramine impairs driving performance as much as or more than a blood alcohol concentration of approximately 0.10%, which exceeds the legal limit in all U.S. states.
When alcohol is added to this equation, impairment becomes even more pronounced.
Studies show that alcohol combined with cognitive distractions produces over-additive impairment at sub-legal blood alcohol levels, meaning the combined deficit is greater than the sum of each factor alone. The same principle applies when mixing alcohol with sedating medications like Benadryl.
Importantly, self-reported drowsiness does not reliably predict objective impairment. You may feel relatively alert while your reaction time, lane-keeping ability, and hazard detection are severely compromised.
This disconnect makes the combination particularly treacherous for activities like driving, operating machinery, or even walking on stairs.
Can You Overdose on Benadryl and Alcohol?
Yes, you can overdose when mixing Benadryl and alcohol, and the risk is higher than with either substance alone.
National poison surveillance data show that intentional diphenhydramine exposures increased 63% between 2005 and 2016, with major adverse clinical effects rising 91% and 745 deaths reported during that period.
Suicide attempts involving diphenhydramine surged dramatically among adolescents and older adults.
When evaluating diphenhydramine toxicity, poison control experts look for specific warning signs that predict severe outcomes.
A multicenter toxicology analysis identified three key predictors of dangerous complications: acidemia (blood pH below 7.2), QRS prolongation on ECG (greater than 120 milliseconds), and elevated anion gap (above 20).
Alcohol co-ingestion can worsen these parameters by impairing protective reflexes, deepening CNS depression, and complicating the clinical picture.
Emergency Thresholds and When to Seek Help
Evidence-based out-of-hospital triage guidelines recommend immediate emergency department referral for any suspected intentional overdose or malicious exposure.
For unintentional ingestions in children under six years, the threshold is 7.5 mg/kg or greater; for those six and older, it is 7.5 mg/kg or 300 mg, whichever is less.
These thresholds apply to diphenhydramine alone. When alcohol is involved, even lower doses warrant medical evaluation due to additive risks.
If you or someone you know has taken a large amount of Benadryl with alcohol, or shows signs like confusion, hallucinations, severe drowsiness, fainting, seizures, or irregular heartbeat, call Poison Control at 1-800-222-1222 or seek emergency care immediately.
Most Common Side Effects of Mixing Benadryl and Alcohol
The most frequently experienced side effects when combining Benadryl and alcohol fall into five categories:
Excessive sedation and psychomotor impairment: Profound drowsiness, slowed reaction time, impaired coordination and balance, dizziness, and worsened driving performance. These effects represent the most common and functionally consequential outcomes in everyday life.
Cognitive and anticholinergic effects: Attention and memory impairment, confusion or delirium (especially in older adults), blurred vision, dry mouth, constipation, and urinary retention. Alcohol can unmask or intensify these central anticholinergic effects.
Increased fall and injury risk: The combination significantly elevates the likelihood of falls and fractures, particularly in older adults, due to combined sedation, balance impairment, and orthostatic hypotension.
Respiratory and cardiovascular risks: In vulnerable populations or with higher doses, the combination can exacerbate sleep-disordered breathing, cause dangerous drops in blood pressure, and progress to serious CNS depression.
Overdose-related toxicities: In severe cases, seizures, anticholinergic delirium, cardiac conduction abnormalities (such as wide QRS complexes), and QTc prolongation can occur, requiring advanced medical management.
Who is Most at Risk?
Who is most at risk for serious complications from these medications and substances depends on age, other drugs being used, and underlying health. Older adults, people taking other CNS depressants, and individuals with chronic conditions all face heightened vulnerability and require extra precautions:
Older Adults
Older adults face particularly high risks when mixing Benadryl and alcohol. The American Geriatrics
Society Beers Criteria categorizes first-generation antihistamines like diphenhydramine as potentially inappropriate medications for people 65 and older due to strong anticholinergic properties and risks of CNS depression, cognitive impairment, and falls.
Age-related changes compound these risks. Diphenhydramine’s half-life can extend from approximately four hours in children to up to 18 hours in older adults, meaning residual effects persist much longer.
Older adults also have reduced alcohol dehydrogenase activity, leading to higher peak alcohol levels and prolonged effects.
A 2025 retrospective cohort review found that alcohol-medication interactions in older adults increase risks for sedation, hypoglycemia, orthostatic hypotension, gastrointestinal bleeding, and liver damage, with some interactions occurring even at low alcohol intake levels.

People Taking Other CNS Depressants
If you take benzodiazepines, opioids, sedative-hypnotics, or gabapentinoids, adding Benadryl and alcohol creates a dangerous “stacking” effect.
Surveillance data from emergency departments show that multiple sedatives are frequently co-implicated in adverse drug events, and the combination can lead to respiratory depression, profound sedation, and overdose.
Individuals with Chronic Conditions
People with respiratory diseases like COPD or sleep apnea, cardiovascular conditions, cognitive impairment, or liver disease face elevated risks.
Those with alcohol use disorder are particularly vulnerable due to chronic alcohol exposure, polypharmacy patterns, and increased baseline risk for delirium and falls.
Long-Term Cognitive Risks
Beyond acute impairment, emerging evidence suggests that cumulative anticholinergic exposure may harm long-term brain health.
A 2025 cross-sectional study of 328,140 inpatient admissions found that each 1% absolute increase in a physician’s first-generation antihistamine prescribing was associated with 8% higher odds of delirium in older adult patients.
Admissions under physicians in the highest prescribing quartile had 41% higher delirium odds compared to the lowest quartile.
Delirium itself is independently associated with long-term cognitive decline and increased mortality.
A systematic review and meta-analysis of six dementia studies involving 645,865 participants reported that anticholinergic drug exposure is associated with increased risk of incident dementia.
While causation cannot be definitively established, the biological plausibility is strong: central cholinergic signaling is critical for memory and attention.
Repeated exposure to first-generation antihistamines, particularly in the context of alcohol use, may accelerate neurocognitive vulnerability over time.
Safer Alternatives to Benadryl
Non-Sedating Antihistamines
Second-generation antihistamines like fexofenadine, cetirizine, and loratadine provide comparable or superior efficacy for allergic rhinitis and urticaria without significant CNS penetration or anticholinergic burden.
In the same driving simulator study that showed diphenhydramine impaired performance worse than high-dose alcohol, fexofenadine produced no measurable impairment compared to placebo.
These medications are safer choices when alcohol exposure is possible and in older adults. Cetirizine can be mildly sedating in some people but is generally far less impairing than first-generation agents.
For Anaphylaxis
Epinephrine remains the first-line, life-saving therapy for anaphylaxis. Antihistamines are adjunctive for cutaneous symptoms and should be non-sedating when possible to minimize CNS adverse effects.
Despite updated guidelines, emergency departments continue to use diphenhydramine in approximately 62% of anaphylaxis and urticaria cases, reflecting a persistent practice gap.

For Sleep Complaints
Chronic use of diphenhydramine as a sleep aid is discouraged. Tolerance develops quickly, anticholinergic burden accumulates, and next-day impairment may persist, especially in older adults.
Non-pharmacologic insomnia treatments like cognitive behavioral therapy for insomnia (CBT-I) are more effective long-term. Alcohol should never be used as a sleep aid due to rebound insomnia and interaction risks.
Practical Guidance: What You Should Do
Do not combine diphenhydramine with alcohol. The combination significantly impairs driving, hazard response, and cognitive function. If you have taken diphenhydramine, avoid alcohol for at least 24 hours. If you have been drinking, do not take diphenhydramine to help you sleep.
Do not drive or operate machinery after taking diphenhydramine, even if you do not feel drowsy. Objective impairment often exceeds subjective awareness.
Check OTC labels carefully. Many “PM” products and nighttime cold formulations contain diphenhydramine. Avoid concurrent alcohol use with any of these products.
Prefer non-sedating antihistamines like fexofenadine, cetirizine, or loratadine for allergies. Consult a clinician if you have liver disease, take other sedatives, or are older than 65.
For older adults and caregivers: Avoid first-generation antihistamines per Beers Criteria. Choose non-sedating alternatives and reassess necessity and duration. Even moderate alcohol can increase adverse drug reaction risk; watch for orthostatic symptoms and falls.
The Bottom Line
Mixing Benadryl and alcohol is unsafe and should be avoided. The combination produces synergistic CNS depression that reliably increases psychomotor impairment, cognitive slowing, and risks for driving incidents, falls, and overdose.
Older adults face particularly high risks due to age-related pharmacokinetic changes, polypharmacy, and vulnerability to delirium and long-term cognitive decline.
Despite clear evidence of harm, clinical practice continues to favor diphenhydramine in many settings, even though safer, equally effective alternatives exist.
The safest approach is to choose non-sedating antihistamines for allergic conditions, avoid alcohol whenever using any sedating medication, and seek medical guidance if you have concerns about interactions.
If you or a loved one is struggling with patterns of mixing medications and alcohol, or if substance use is affecting your health and safety, professional support can help.
At MARR, we understand the complexities of addiction and co-occurring mental health challenges. Our evidence-based programs combine proven therapies with a supportive community to help you build lasting recovery. Reach out to our team to learn how we can support your journey to health and wellness.
