Many people ask if it is safe to drink alcohol while taking clonidine for blood pressure or other conditions.
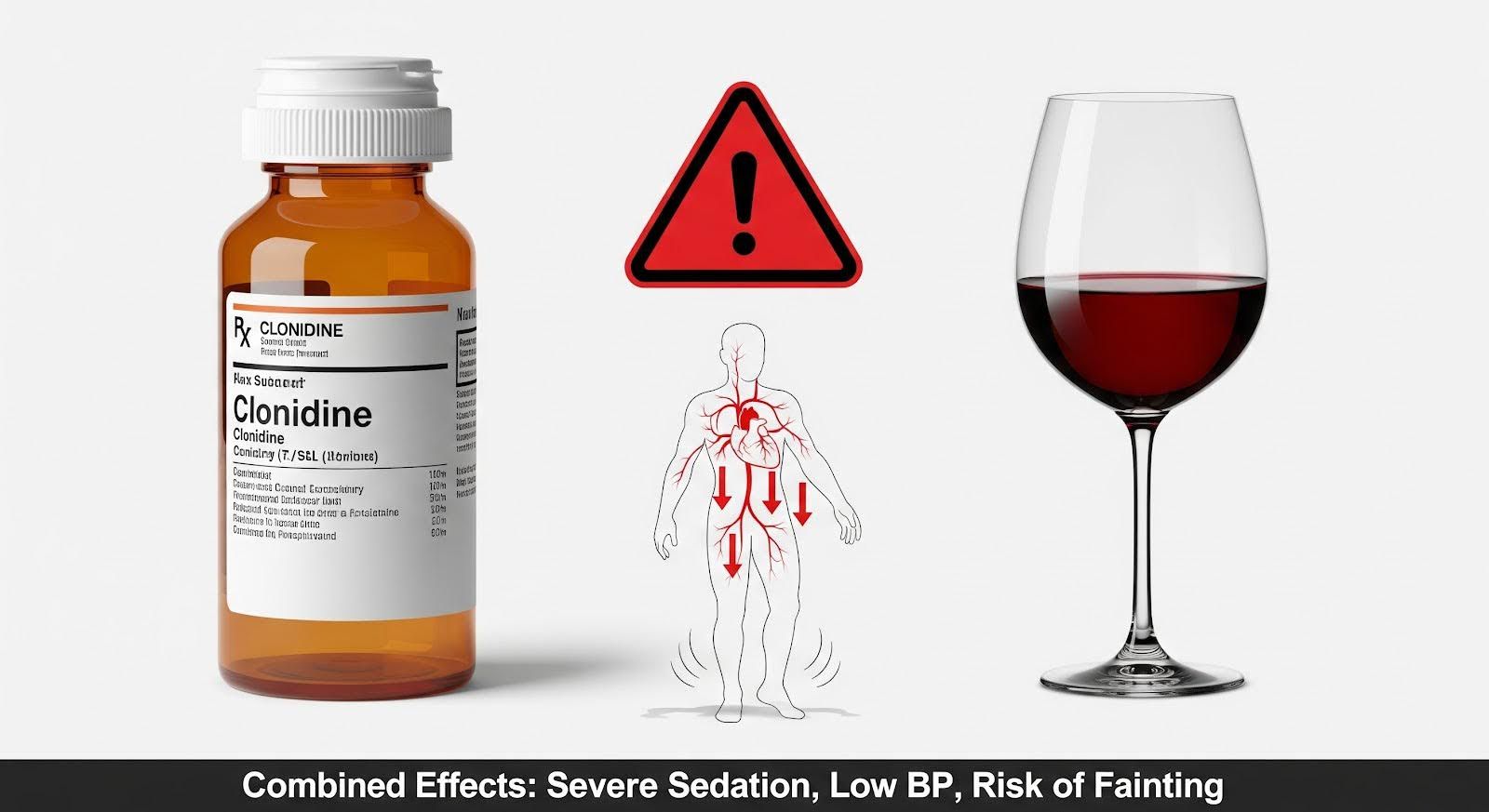
Mixing clonidine and alcohol is dangerous because the combination amplifies sedation and can drop blood pressure to unsafe levels.
This article explains the serious risks of this interaction and how to stay safe.
Clonidine and Alcohol Interaction Risks
Clonidine is a medication primarily used to treat high blood pressure (hypertension) and attention-deficit/hyperactivity disorder (ADHD).
It works by relaxing blood vessels and reducing the heart rate. Alcohol is a central nervous system (CNS) depressant that slows down brain activity.
When you mix clonidine and alcohol, the effects of both substances do not just add up; they multiply.
This creates a synergistic effect where the sedation and physical impairment are much stronger than what you would experience with either substance alone.
The primary danger lies in the impact on your heart and brain. Clonidine lowers your heart rate and blood pressure, and alcohol expands your blood vessels, which can lower blood pressure further. This combination can lead to severe dizziness, fainting, and a risk of falls.
The Mechanism Behind the Risk
Clonidine works as a central alpha-2 adrenergic agonist. This means it blocks specific signals from the brain to the nervous system that normally keep your heart rate and blood pressure up.
Alcohol also depresses the central nervous system. When these two mechanisms overlap, the body loses its ability to regulate blood pressure effectively.
Research indicates that this interaction causes synergistic CNS depression, meaning the drowsiness and lack of coordination are far more intense than expected.
This can be particularly risky for people who drive or operate machinery, as the level of impairment can occur rapidly and without warning.
Impact on Heart Rate and Blood Pressure
The combination of clonidine and alcohol creates a dual threat to your cardiovascular stability. Clonidine naturally causes bradycardia, which is a slower than normal heart rate.
Alcohol can cause peripheral vasodilation, where blood vessels widen and blood pressure drops.
When taken together, these effects heighten the risk of clinically significant hypotension (dangerously low blood pressure).
This can result in syncope, which is a medical term for fainting or passing out. If a person faints while intoxicated, they are at a higher risk of injury from falling or aspirating vomit, which can be fatal.
Side Effects of Mixing Alcohol and Clonidine
The side effects of mixing alcohol and clonidine range from mild discomfort to life-threatening emergencies.
Because both substances affect the brain’s alertness levels, the most immediate sign of an interaction is profound drowsiness. However, the physical symptoms can escalate quickly.
Common side effects include:
- Extreme drowsiness or lethargy
- Dry mouth
- Dizziness and lightheadedness
- Slowed reflexes and impaired judgment
- Unsteadiness or loss of coordination
In more severe cases, the interaction leads to dangerous outcomes that may require emergency medical attention.
The risk of respiratory compromise increases, meaning breathing may become shallow or stop altogether. This is especially true if other depressants, such as opioids or benzodiazepines, are also involved.
Comparing the Effects
Understanding the difference between the effects of the drug alone versus the combination can help identify when an interaction is occurring.
| Feature | Clonidine Alone | Alcohol Alone | Clonidine + Alcohol |
| Primary Effect | Lowers BP/HR, sedation | Sedation, incoordination | Profound sedation, dangerously low BP |
| Heart Rate | Slows down (bradycardia) | Variable, often unchanged | Markedly slower; high risk of fainting |
| Mental State | Calm, sleepy | Impaired judgment | Hard to arouse, confusion, deep stupor |
| Physical Risk | Dizziness when standing | Poor balance, stumbling | Severe fall risk; high chance of head injury |
Clonidine and Alcohol Withdrawal Management
Clonidine is frequently used in medical settings to help manage alcohol withdrawal syndrome (AWS).
However, its role is specific and limited. It is used as an adjunct treatment, meaning it is added to other primary medications rather than being the main treatment itself.
The Role of Clonidine in Detox
During alcohol withdrawal, the body experiences a surge of adrenaline, leading to symptoms like sweating, tremors, rapid heart rate, and high blood pressure.
Clonidine helps dampen this autonomic hyperactivity, making the patient more comfortable.
It is important to note that clonidine does not prevent seizures or delirium tremens, which are the most dangerous complications of alcohol withdrawal.
For this reason, benzodiazepines remain the first-line treatment for preventing these severe outcomes. Clonidine is only added when heart rate and blood pressure remain high despite standard treatment.

Risks During Withdrawal Treatment
Using clonidine for alcohol withdrawal requires careful medical supervision. Because the patient may still have alcohol in their system or may be receiving benzodiazepines, adding clonidine increases the risk of over-sedation.
Clinicians must monitor the patient closely to ensure that the medication does not hide worsening symptoms.
For example, a rising heart rate is often a sign that withdrawal is getting worse. If clonidine artificially lowers the heart rate, medical staff might miss the warning signs of an impending seizure.
Therefore, clinical guideline highlights advice against using clonidine as a standalone therapy for alcohol withdrawal.
Dangers of Clonidine and Alcohol Interaction in Special Groups
Certain groups of people face much higher risks when mixing clonidine and alcohol.
Physiological changes due to age or health conditions can make the body less able to process these substances, leading to toxic buildup and more severe reactions.
Older Adults
Older adults are particularly vulnerable to the side effects of clonidine, even without alcohol.
The Beers criteria list clonidine as a potentially inappropriate medication for older adults due to the high risk of profound bradycardia and hypotension.
When alcohol is added, the risk of falls and hip fractures increases dramatically. Older kidneys also process drugs more slowly, meaning the medication stays in the system longer.
This extended duration means that even a small amount of alcohol can trigger a significant adverse event, such as fainting upon standing.
Renal Impairment
People with kidney disease or those on dialysis must be extremely cautious. Clonidine is removed from the body through the kidneys.
In patients with renal impairment, the drug’s half-life can extend from the typical 12 hours to over 40 hours.
Because clonidine is not appreciably dialyzable, it cannot be easily removed from the blood if an overdose or bad interaction occurs.
Alcohol use in this population can lead to unpredictable blood pressure fluctuations and dangerous accumulation of the drug, leading to extended periods of sedation and instability.

Pediatric Risks
While children do not typically consume alcohol intentionally, the presence of clonidine in the home for ADHD treatment has led to a rise in accidental poisonings. Poison center data shows that pediatric exposures to clonidine are increasing.
In adolescents who may experiment with alcohol, the combination is perilous. A young person taking clonidine for ADHD who drinks alcohol may experience a rapid onset of deep sedation and slow heart rate, which can be mistaken for simple drunkenness, delaying necessary medical help.
Overdose and Emergency Management
Recognizing the signs of a clonidine and alcohol overdose can save a life. The window for intervention can be short, especially if the person has passed out.
Identifying an Overdose
The hallmark signs of toxicity involving clonidine include a very slow heart rate (bradycardia), low blood pressure (hypotension), and pinpoint pupils. When alcohol is involved, the person may be unable to wake up.
Breathing may become shallow or irregular. In severe cases, the person may require mechanical ventilation because their body forgets to breathe.
If you suspect someone has mixed these substances and cannot be awakened, call emergency services immediately.
Medical Treatment
There is no specific antidote that completely reverses clonidine poisoning. Treatment focuses on supportive care. Doctors will focus on keeping the airway open and maintaining blood pressure.
Intravenous fluids are often given to boost blood pressure. If that is not enough, medications called vasopressors may be used to tighten blood vessels.
While naloxone is sometimes used in pediatric clonidine toxicity to reverse sedation, it is not always effective and is used with caution in adults who might also be dependent on opioids.
Why Does It Matter?
Understanding the interaction between clonidine and alcohol is not just about avoiding a bad hangover; it is about preventing life-threatening medical emergencies.
The combination creates a perfect storm of depressed brain function and cardiovascular instability.
For patients prescribed clonidine, the safest choice is to avoid alcohol completely.
If you are taking clonidine for alcohol withdrawal, it is vital to do so only under strict medical supervision where your heart rate and blood pressure can be monitored constantly. The risks of falls, head injuries, and respiratory failure are too high to ignore.
If you or a loved one are struggling to manage alcohol use while taking medication, MARR’s professional support can ensure safety and stability.
