When someone survives an overdose and arrives at an Atlanta emergency room, the next hours and days are critical.
Many families wonder whether their loved one will receive help connecting to addiction treatment before leaving the hospital.
A national study of Medicare patients found that only 4.1% of overdose survivors received medication for opioid use disorder within 12 months, and 17.4% experienced another nonfatal overdose.
Atlanta hospitals are working to change that pattern through peer recovery coaches and emergency department buprenorphine programs.
This article examines the evidence on how many overdose patients in Atlanta enter treatment after an ER visit, what drives successful linkage, and where gaps remain.
What Percentage of Atlanta Overdose Patients Enter Treatment After an ER Visit?
No official, citywide metric tracks exactly how many Atlanta overdose patients enter treatment after an emergency department visit. Georgia’s public health surveillance captures overdose encounters but does not publish patient-linked treatment initiation rates.
However, program data from Grady Memorial Hospital, Atlanta’s largest emergency department and only Level I trauma center, provide concrete evidence of referral volumes and engagement.
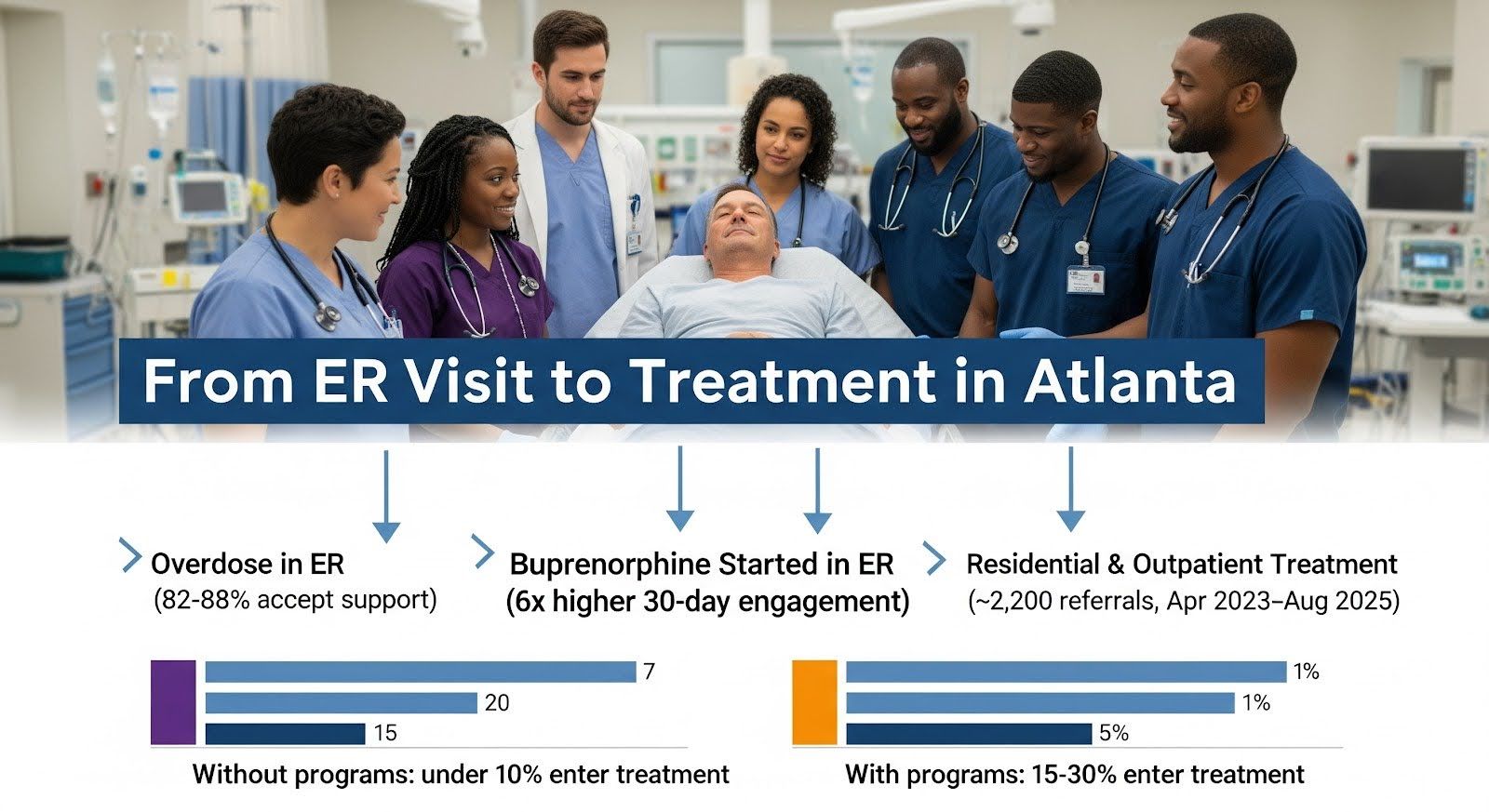
Between April 2023 and late July 2025, Grady’s peer recovery coaching program engaged 2,587 emergency department and hospital patients with substance use disorders, with 82 to 88% accepting linkage support.
More than 700 were placed directly into residential treatment, and many others were referred to outpatient medication and counseling services.
Based on these figures and Grady’s central role in Atlanta’s overdose response, a defensible estimate is that approximately 2,200 ER patients in Atlanta were referred to addiction treatment from April 2023 through August 2025, with overdose survivors representing a substantial share of these referrals.
National evidence suggests that 15 to 30% of overdose patients enter any addiction treatment within 30 days of an ER visit when hospitals implement peer recovery and medication-assisted treatment programs.
Sites without these programs see rates below 10%. Atlanta’s performance likely falls within this range, with higher engagement at hospitals using structured linkage pathways and lower rates elsewhere.
The Evidence for Emergency Department Buprenorphine and Peer Recovery
Randomized trials demonstrate that starting buprenorphine in the emergency department dramatically improves treatment engagement.
A systematic review published in 2025 found that ED-initiated buprenorphine increased 30-day treatment engagement by nearly six times compared to referral alone, with precipitated withdrawal occurring in less than 1% of cases.
Retention remains highest in the first 24 hours (77%) but declines over time, underscoring the importance of rapid follow-up after discharge.
Peer recovery coaches complement medication by providing motivational support, scheduling appointments, and helping patients navigate insurance and transportation barriers.
The combination of same-day buprenorphine and peer-facilitated warm handoffs to outpatient care represents the most effective strategy for converting an overdose ER visit into sustained treatment engagement.
Atlanta’s Emergency Department Linkage Infrastructure
Grady Memorial Hospital operates the LINCS UP program, funded by the Centers for Disease Control and Prevention, which deploys peer recovery coaches in the emergency department and inpatient units.
Coaches offer both in-person and telehealth support and continue contact after discharge. The program reports seeing approximately 90 patients per month and has maintained an 84% engagement agreement rate since inception.
Grady’s emergency department also has 24/7 access to an Emory Addiction Medicine consultation service, which supports initiation of buprenorphine for patients in opioid withdrawal.
Patients can then transition to the Medication for Alcohol and Opioid Treatment clinic, which provides outpatient buprenorphine, extended-release naltrexone, counseling, and peer support at no cost for uninsured individuals.
Emory Healthcare and Grady have expanded peer recovery coaching and naloxone distribution in emergency and inpatient settings using opioid settlement funds, with plans to extend services to Emory Midtown.
Why Many Overdose Patients Still Miss Treatment?
Despite these programs, most Atlanta overdose patients do not enter treatment within 30 days of an ER visit. Several factors explain the gap:
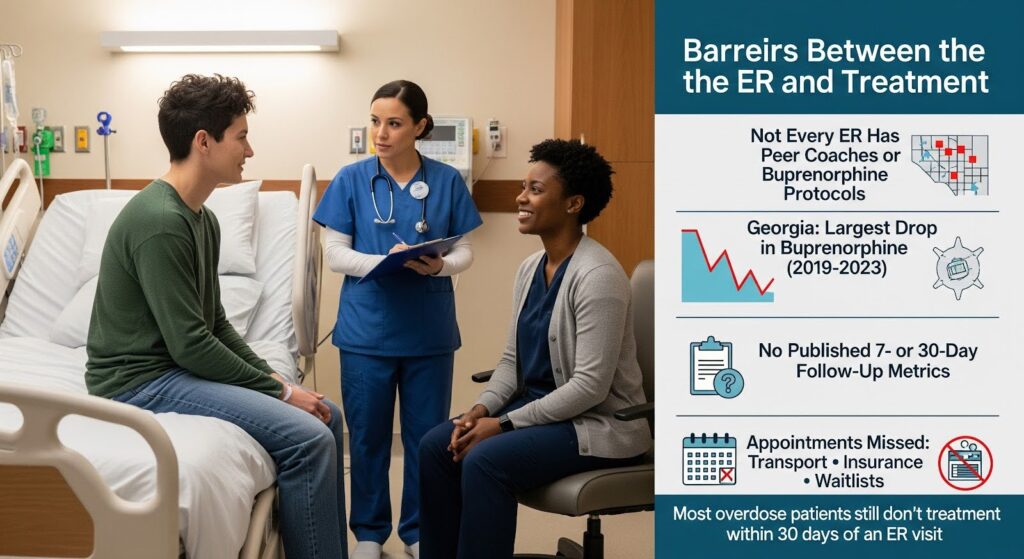
- Uneven adoption across hospitals: Not all Atlanta emergency departments have peer recovery coaches or protocols for initiating buprenorphine. Patients treated at hospitals without these resources are far less likely to connect to care.
- Georgia’s buprenorphine access challenges: A 2019 to 2023 analysis found Georgia experienced the largest decline in buprenorphine distribution among all states, indicating systemic barriers that depress medication uptake even when patients are referred.
- Measurement gaps: Georgia does not publish patient-linked metrics showing how many overdose patients enter treatment within 7 or 30 days of an ER visit, making it difficult to track performance and hold systems accountable.
Follow-up falls through the cracks: Even when patients accept referrals, they may not attend the first appointment due to transportation problems, insurance delays, or lack of immediate availability at treatment programs.
Measuring What Matters: The Follow-Up After Emergency Department Visit Metric
The National Committee for Quality Assurance developed a measure called Follow-Up After Emergency Department Visit for Substance Use, which tracks the percentage of patients who receive addiction care within 7 or 30 days of an ER visit for substance use or overdose.
The measure counts outpatient visits, telehealth encounters, and medication dispensing events as successful follow-up.
Georgia Medicaid managed care plans are required to report this measure, but the state does not publish city-level dashboards showing Atlanta’s performance.
The Centers for Medicare and Medicaid Services retained April 30 as the annual reporting deadline for external quality reviews, even though audits typically finalize in June, creating timing misalignment that delays public visibility into follow-up rates.
Publishing Atlanta-specific 7-day and 30-day follow-up rates, stratified by hospital and demographic group, would provide transparent accountability and help identify which emergency departments need additional peer recovery and medication resources.
Surveillance Capacity and Data Linkage Opportunities
Georgia participates in the CDC’s Enhanced State Opioid Overdose Surveillance program, which improves timeliness and completeness of emergency department and EMS nonfatal overdose data.
The state also mandates electronic patient care reporting from EMS agencies using the NEMSIS version 3.5 standard, creating a structured prehospital data pipeline.
These surveillance systems capture overdose encounters but are not currently linked to treatment claims or health system records to produce patient-level follow-up metrics.
Connecting emergency department syndromic surveillance, prescription drug monitoring program data, and Medicaid claims would enable Georgia to calculate and publish the percentage of overdose patients entering treatment after an ER visit, similar to how states track other care transitions.
What Drives Successful Linkage to Treatment?
Research and program experience point to several key elements:
- Same-day buprenorphine initiation: Starting medication in the emergency department, rather than waiting for an outpatient appointment, increases the likelihood that patients will engage in ongoing treatment.
- Peer recovery coaches: Trained peers with lived experience build trust, provide hope, and help patients navigate logistical barriers that often derail referrals.
- Warm handoffs: Scheduling the first outpatient appointment before the patient leaves the hospital, ideally within 24 to 72 hours, prevents loss to follow-up.
- No-cost or low-barrier access: Programs like Grady’s MAOT clinic, which provides buprenorphine at no cost for uninsured patients, remove financial obstacles that prevent treatment entry.
- Naloxone distribution: Sending every overdose patient home with naloxone and overdose education reduces the risk of fatal overdose while they are waiting to start treatment or if they experience a recurrence.
| Linkage Strategy | Impact on 30-Day Engagement | Implementation Requirement |
| ED-initiated buprenorphine | 6-fold increase vs referral only | Trained prescribers; pharmacy stocking; consult service |
| Peer recovery coaching | 82–88% accept linkage support | Peer workforce; supervision; workflow integration |
| Warm handoff to bridge clinic | High early retention (77% at 24 hours) | Rapid-access outpatient slots; care coordination |
| Naloxone distribution | Reduces fatal overdose risk | Supply chain; patient education; standing orders |
Why Does This Matter for Families and Communities?
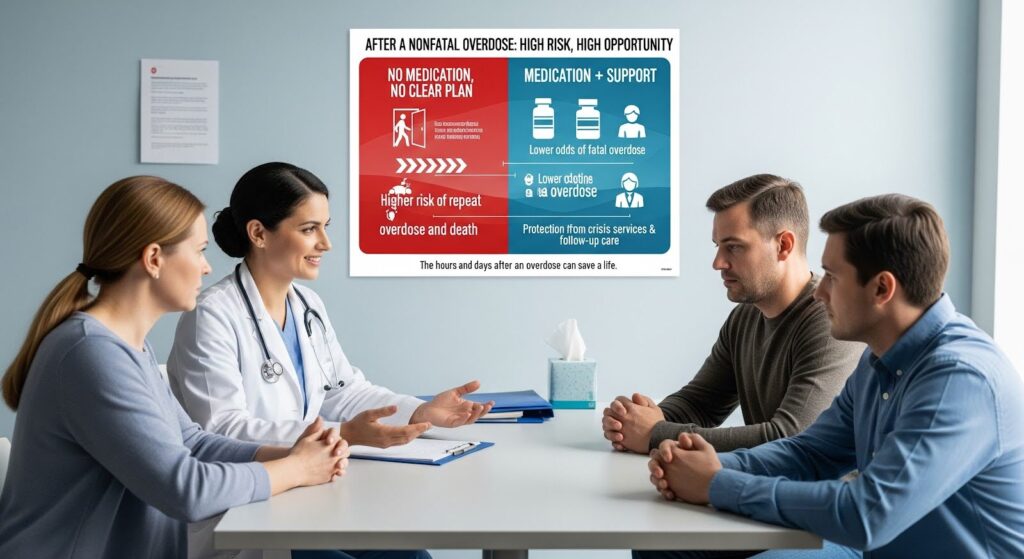
The period after a nonfatal overdose is a window of both high risk and high opportunity.
National data show that methadone and buprenorphine are strongly associated with lower odds of fatal overdose, while behavioral health assessment and crisis services after an ER visit also provide significant protection.
Conversely, patients who leave the emergency department without medication or a clear path to treatment face elevated risk of repeat overdose and death.
For families, knowing that Atlanta hospitals are investing in peer recovery coaches and medication programs offers hope.
At the same time, the absence of citywide metrics and uneven implementation across emergency departments means that outcomes depend heavily on which hospital a loved one reaches.
Standardizing peer recovery and buprenorphine initiation across all Atlanta emergency departments would ensure that every overdose survivor has an equal chance to enter treatment.
Next Steps for Atlanta’s Overdose Response
To increase the percentage of overdose patients who enter treatment after an ER visit, Atlanta can take several concrete actions:
- Expand peer recovery coaching: Scale the LINCS UP model to all major emergency departments in the metro area, with both in-person and telehealth capacity.
- Standardize ED-initiated buprenorphine: Adopt protocols at every hospital for starting buprenorphine in the emergency department, supported by 24/7 addiction medicine consultation and pharmacy stocking.
- Publish transparent metrics: Create a public dashboard reporting 7-day and 30-day treatment linkage rates for overdose patients, stratified by hospital, insurance type, race, and ethnicity.
- Link surveillance and claims data: Use Georgia’s Enhanced State Opioid Overdose Surveillance infrastructure and Medicaid managed care claims to calculate patient-linked follow-up rates.
- Address pharmacy access: Work with community pharmacies to ensure buprenorphine is stocked and dispensed promptly, reducing delays that cause patients to disengage.
Conclusion
Approximately 2,200 emergency room patients in Atlanta were referred to addiction treatment from April 2023 through August 2025, largely through Grady Memorial Hospital’s peer recovery coaching program.
While this represents meaningful progress, the majority of overdose patients across the metro area still do not enter treatment within 30 days of an ER visit.
National evidence shows that 15 to 30% engagement is achievable when hospitals implement peer recovery and medication-assisted treatment programs, but Atlanta lacks the citywide data needed to track performance and drive improvement.
The most effective interventions, starting buprenorphine in the emergency department, deploying peer recovery coaches, and ensuring warm handoffs to outpatient care, are proven to save lives.
Expanding these practices across all Atlanta emergency departments and publishing transparent, equity-focused metrics would convert more overdose ER visits into sustained recovery pathways.
If someone you care about is struggling with addiction, MARR’s professional treatment can provide the structure and support needed for lasting change.
