Relapse after treatment is one of the most painful setbacks in recovery. Within 90 days of leaving structured care, many people return to regular use, and the risk varies sharply by substance.
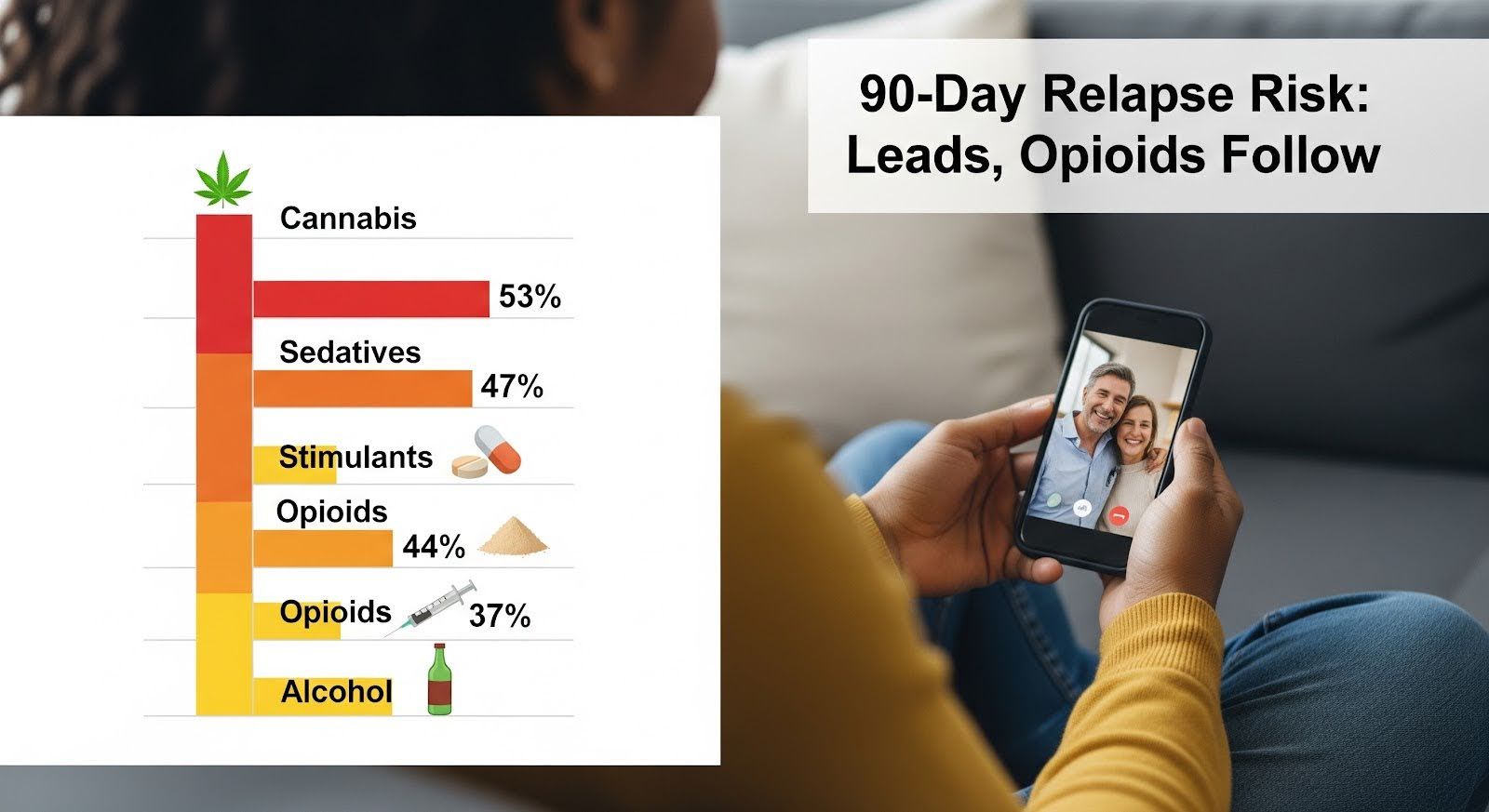
A recent study of inpatients with co‑occurring psychiatric disorders found that cannabis users relapsed at the highest rate, 53%, followed closely by sedatives at 47%, stimulants at 44%, and opioids at 44%.
This article explains which drugs carry the greatest 90‑day relapse risk, what triggers drive early return to use, and which treatment strategies can protect you during the most vulnerable window.
Cannabis and Sedatives Lead 90‑Day Relapse Rates
When researchers tracked inpatients with both substance use disorders and mental health conditions for three months, cannabis users relapsed most often, with more than half returning to regular use, defined as two to four times per week or more.
Sedative users were close behind at 47%, while stimulant and opioid users both relapsed at 44%. Alcohol showed a lower but still substantial rate of 37%.
These findings challenge the common assumption that opioids always top the relapse list. In this population, cannabis and sedatives posed the highest short‑term risk.
The presence of a co‑occurring psychiatric disorder amplified relapse across all substances, roughly doubling the odds for cannabis and stimulant users compared to those without mental health diagnoses.
Why Cannabis Relapse is So Common?
Cannabis is often perceived as less harmful, which can lead to underestimating relapse risk. Yet the data show that people with cannabis use disorder and a mental health condition face the steepest climb in early recovery.
Older age, being female, and higher motivation to change all reduced relapse risk, but cannabis and stimulant diagnoses still carried odds ratios around 2.1 to 2.3 in this group.
Opioid Relapse Risk Depends on Your Treatment Path
For opioid use disorder, the 90‑day picture is more complex. Relapse rates hinge on whether you receive medication for opioid use disorder or detox alone.
Studies show that roughly one‑quarter of patients relapse on the day they leave detox, and about 65% relapse within the first month. Those who do not start MOUD or enter residential treatment in that first month face the highest 12‑month mortality, around 2%.
In contrast, starting buprenorphine during residential care lowers illicit opioid use at 12, 35, 95, and 185 days compared to withdrawal management alone.
The fentanyl era has made this even more urgent: reduced tolerance after detox combined with high‑potency street opioids creates a deadly window. Relapse proportions in some studies reached as high as 95% within six months when patients did not receive ongoing medication.
Stimulant Co‑Use is the Strongest Near‑Term Trigger
Among people on MOUD, concurrent stimulant use, methamphetamine, amphetamines, or cocaine, is the most powerful predictor of return to opioid use.
Pooled trial data show that time‑varying stimulant use raised the hazard of first opioid use more than ninefold overall, with an even stronger effect on buprenorphine (13‑fold) than on extended‑release naltrexone (nearly fivefold).
Each additional day of stimulant use in a seven‑day window increased hazard by 27%, and weekly or more frequent stimulant use doubled the odds of progressing from a single lapse to ongoing relapse.
This means that for opioid users, the question “which drug has the highest relapse risk at 90 days” often depends on what else you are using. Stimulant co‑use can overwhelm the protective effect of medication, especially buprenorphine, making integrated treatment for both substances essential.
Depression Accelerates Early Relapse Across Substances
Major depressive disorder shapes relapse risk in distinct ways. Substance‑induced depression, episodes triggered by intoxication or withdrawal, strongly predicts earlier first use after discharge.
Hazard ratios ranged from 4.7 for alcohol to 6.5 for heroin, meaning people with substance‑induced depression were four to six times more likely to use soon after leaving treatment.
Independent depression, which exists apart from substance use, increases relapse hazards for alcohol and cocaine once someone has achieved sustained remission, at least 26 weeks symptom‑free.
It also reduces the likelihood of reaching sustained remission for cocaine and heroin in the first place. In one MOUD cohort, higher depression scores predicted a positive opioid urinalysis at 90 days, while older age predicted better engagement.
Treating Depression is Part of Relapse Prevention
These findings underscore that depression care is not optional. Screening for both substance‑induced and independent depression, then treating each aggressively with therapy and medication, can protect early remission and reduce the chance of relapse within the first three months.
The Fentanyl Era Compounds Relapse Vulnerability
The drug supply has changed dramatically. Fentanyl and its analogues now dominate the illicit opioid market, and stimulant–opioid co‑use has become more common and persistent.
A longitudinal cohort study found that people who reported co‑use were most likely to continue that pattern over time, and co‑use was associated with homelessness, incarceration, depressive symptoms, and the highest probability of fatal overdose.
This “stickiness” of polysubstance use, combined with social instability and mental health challenges, creates a high‑velocity relapse environment.
The first 90 days after treatment are especially dangerous because tolerance drops during abstinence, and even a small amount of fentanyl can be lethal.
Key Relapse Triggers and Protective Factors at 90 Days
| Trigger or Factor | Effect on Relapse Risk | What it Means |
|---|---|---|
| Stimulant use during MOUD | Hazard ratio ≈9.2 overall; ≈13.1 on buprenorphine | Most potent near‑term trigger for opioid relapse |
| Substance‑induced depression | Hazard ratios ≈4.7–6.5 for first use | Accelerates early lapse across alcohol, cocaine, heroin |
| Independent depression | Hazard ratios ≈2.3–2.7 for relapse after remission | Increases relapse for alcohol and cocaine |
| Detox without MOUD or residential care | ≈25% relapse day of discharge; ≈65% within one month | Highest mortality if no treatment in first month |
| Younger age | Increased relapse at 3 months | Prioritize retention and supports for younger patients |
| Treatment completion | Protective | Completing inpatient stay lowers relapse risk |
| Co‑occurring psychiatric disorder | Roughly doubles relapse odds for cannabis and stimulants | Screen and treat mental health conditions |
What Works to Reduce Relapse in the First 90 Days?
The evidence points to several high‑impact strategies:
Start and continue medication for opioid use disorder. Buprenorphine induction during residential care reduces illicit opioid use at 95 days and beyond. Detox alone is unsafe and ineffective; more than 90% may return to use within months. Initiating MOUD or residential treatment in the first month after detox is highly protective.
Address stimulant co‑use proactively. Screen weekly for stimulant use in MOUD patients and deploy contingency management, a behavioral intervention that rewards drug‑free urine tests, to reduce stimulant exposure and blunt progression from lapse to ongoing relapse.
Treat depression systematically. Identify and treat both substance‑induced and independent depression with pharmacotherapy and psychotherapy. Expect accelerated first use with substance‑induced episodes and higher relapse hazards for alcohol and cocaine with independent depression.
Secure early aftercare and psychosocial supports. Completing the initial inpatient or residential stay and linking to outpatient care within seven days lowers relapse risk. Address homelessness and legal issues through coordinated case management to disrupt persistent co‑use patterns.
Extend treatment duration and retention. Longer programs, more than six months, are protective compared to short‑term stays of two to four months. Retention in treatment for at least 90 days is a widely used benchmark linked to improved outcomes.

Why Measurement Matters for Understanding Relapse?
One reason relapse rates vary so widely across studies is that “relapse” is defined inconsistently. Some studies count any use, others require a return to regular use, and still others look for three consecutive positive urine tests or readmission to a higher level of care.
Follow‑up windows range from one week to six months, and measurement methods include self‑report, biological confirmation, chart notes, and administrative data.
This heterogeneity makes it hard to compare relapse rates across substances at a fixed point like 90 days. The most reliable comparisons come from studies that use the same definition, population, and timeframe.
The inpatient co‑occurring disorder cohort cited here used a uniform “return to regular use” threshold at three months, which is why its substance‑by‑substance rankings are credible.
Future research should standardize 30‑, 60‑, and 90‑day relapse definitions, combine self‑report with biological confirmation, and use time‑to‑event models like Cox proportional hazards to estimate early hazard and capture recurrent events.
These steps will improve cross‑substance comparisons and help clinicians and programs target the highest‑risk periods more precisely.
The Bottom Line on 90‑Day Relapse Risk
Among inpatients with co‑occurring psychiatric disorders, cannabis and sedatives carry the highest relapse risk at 90 days, followed closely by stimulants and opioids, with alcohol lower but still substantial.
For opioid use disorder specifically, relapse risk depends heavily on treatment pathway: detox alone leads to extremely high early relapse and elevated mortality, while MOUD reduces risk, though concurrent stimulant use remains a powerful trigger that can overwhelm medication’s protective effect.
Depression is a central driver across substances, accelerating first use when substance‑induced and increasing relapse hazards for alcohol and cocaine when independent.
In the fentanyl era, persistent stimulant–opioid co‑use, social instability, and psychiatric comorbidity create a high‑velocity relapse ecosystem that demands integrated clinical, social, and pharmacologic responses.
The most impactful 90‑day strategies are clear: avoid detox‑only pathways, initiate and retain MOUD for at least 90 days, proactively detect and treat stimulant co‑use with evidence‑based behavioral interventions, systematically evaluate and treat depression, and secure early aftercare and psychosocial supports.
These steps collectively shift patients off the early‑relapse trajectory and are essential for improving outcomes across all substances.
If you or someone you care about is navigating early recovery, know that the first 90 days are both the most vulnerable and the most important. With the right supports in place, relapse is not inevitable.
Reach out to our trusted provider to discuss medication options, behavioral therapies, and the structure you need to protect your progress. Consider exploring MARR addiction counseling to build a personalized plan that addresses your unique risks and strengths during this critical window.
