Women entering addiction treatment face distinct challenges that can shape their recovery journey.
Research shows that about 11% of ever-partnered women experience intimate partner violence in a given year, and many carry trauma histories that complicate treatment.
The strongest predictors of lasting recovery in gender-specific programs are not the women-only format itself but rather sustained engagement in treatment and ongoing participation in mutual-help groups after discharge.
Programs that remove barriers like childcare gaps, unsafe housing, and partner substance use exposure see better retention and outcomes over 12 to 24 months. This article explains which factors drive long-term success and how gender-responsive design can improve results.
Why Gender-Specific Treatment Matters?
Women entering substance use disorder treatment often report higher rates of childhood trauma, intimate partner violence, child welfare involvement, and financial dependence compared to men.
These overlapping challenges create barriers to access and retention, supporting the rationale for gender-responsive services that address safety, parenting, and social stability alongside addiction symptoms.
Trauma-informed care, childcare support, and less confrontational group formats are examples of responsive features that can improve engagement.
Despite evidence of distinct needs, specialized services remain limited. Only about one-third of facilities offer women’s programs, fewer than 10% provide childcare, and just 4% offer beds for children.
This service gap persists even as research shows that gender-responsive adaptations can enhance retention and outcomes for certain subgroups, particularly women with high psychiatric severity or complex trauma histories.
Retention and Length of Stay Drive Outcomes
Across multiple studies, longer time in treatment robustly predicts abstinence and reduced criminal activity at 12 months for both women and men.
This factor may mediate the benefit of gender-responsive features that increase attendance and reduce early dropout. Put differently, gender-responsive design primarily enhances outcomes by improving retention and continuity of care.
A comparative study of 291 women in outpatient programs found that both women-only and mixed-gender settings produced improvements across drug and alcohol use, criminal activity, arrests, and employment at one year.
The comparative results were mixed, indicating that women-only care is not uniformly superior across outcomes.
Women-only programs employed similar core components to mixed-gender care but emphasized supportive, less confrontational group dynamics and contextualized content for women’s recovery needs.
What Keeps Women Engaged?
Gender-responsive features that improve retention include:
- Onsite childcare or residential options allowing mothers to live with children
- Trauma-informed therapy and safety planning
- Flexible scheduling and transportation support
- Integrated case management addressing legal, housing, and health needs
- Supportive group processes that reduce shame and confrontation
These elements lower practical barriers and create an environment where women can stay long enough for treatment to take hold.
Mutual-Help Participation Extends Gains Beyond Discharge
Participation in 12-step groups correlates with abstinence at follow-up for both genders, with evidence of dose-response effects. Greater duration and frequency of Alcoholics Anonymous participation predicts more favorable long-term outcomes in alcohol use disorders.
Complementary work shows that intensive referral to 12-step can improve one-year outcomes for some populations, though effects vary by subgroup and implementation fidelity.
A randomized trial among 66 women veterans with severe substance use disorder compared a gender-focused model to 12-Step Facilitation. Both arms showed significant reductions in substance use from baseline to end-of-treatment and to three-month follow-up, with large effect sizes for alcohol and medium effects for other drugs.
Importantly, there were no differences between the two approaches on primary outcomes, and 12-step attendance did not increase in either arm. This finding underscores that formal facilitation does not guarantee increased mutual-help participation and that sustained post-treatment engagement remains a distinct implementation challenge.
A 2018 to 2021 machine-learning analysis identified two primary predictors of treatment success: attending self-help groups while in treatment and setting specific treatment goals.
Secondary predictors that facilitate these behaviors include linkage to a primary care provider and access to social supports like SNAP.
Although not specific to women, these proximal drivers align with core mechanisms in mutual-help literature and with gender-responsive care that lowers practical barriers such as childcare, flexible scheduling, and transportation to attend meetings and pursue goals.
Gender-Differentiated Predictors at 12 Months
At 12 months, longer retention predicts abstinence and crime desistence for both men and women, but baseline predictors differ by gender.
For women, multiple drug use and readiness for treatment predicted abstinence, and legal involvement plus readiness predicted crime desistence. For men, spousal drug use predicted abstinence, and legal involvement, multiple drug use, and living with children predicted crime desistence.
For both genders, participation in 12-step groups and absence of spousal drug use during follow-up correlated with abstinence at one year.
These gender-differentiated predictors suggest that gender-specific programming should emphasize motivational enhancement and multi-substance stabilization for women, and address partner substance use exposures for both genders.
Assessment and active management of partner risk exposure, such as couples-based interventions where safe or safety planning in contexts of intimate partner violence, become crucial components of gender-specific recovery plans.
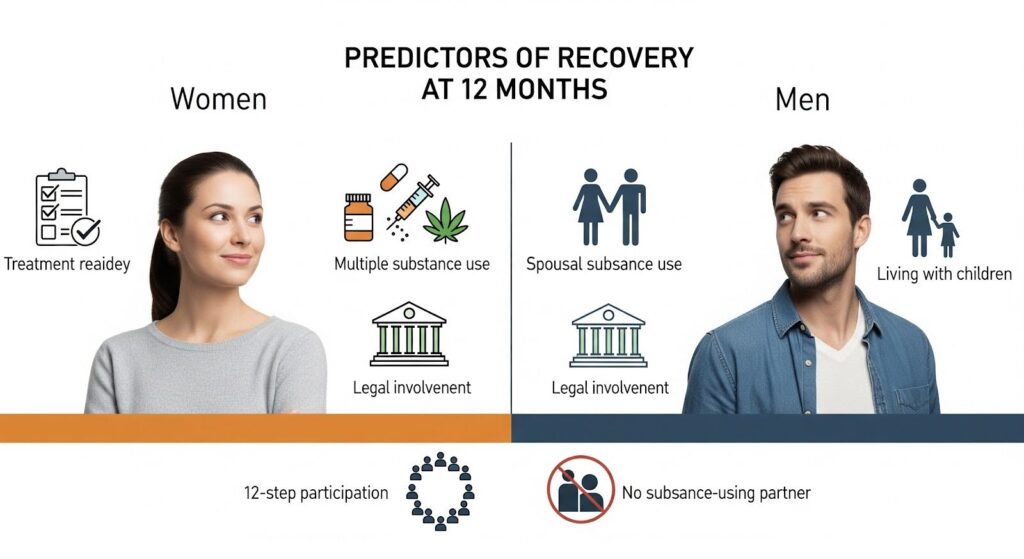
| Outcome | Women Predictors | Men Predictors | Common to Both | Implications |
|---|---|---|---|---|
| Abstinence at 12 months | Multiple drug use (negative); readiness for treatment (positive) | Spousal drug use (negative) | Longer retention; 12-step participation; absence of spousal drug use | For women: emphasize motivational enhancement and multi-substance stabilization; for both: address partner-related risk and support mutual-help engagement |
| Crime desistence at 12 months | Legal involvement; readiness for treatment | Legal involvement; multiple drug use; living with children | Longer retention | Leverage structured accountability; integrate family and parenting supports; reduce instability to improve retention |
Program Design Features That Work
Standard mixed-gender outpatient programs typically combine individual and group counseling, vocational and educational components, 12-step meetings, peer discussions, and random urine testing.
Average time in treatment approximates seven months in some cohorts, indicating substantial exposure during follow-up. Retention in such programs is a strong prognostic indicator.
Women-only programs often include the same core components but contextualize content for women, such as parenting stress, intimate partner violence dynamics, and trauma responses.
They emphasize supportive, less confrontational group approaches and incorporate wraparound services when possible, including childcare, legal assistance, and mental health integration.
Comparative studies show mixed outcome differences versus mixed-gender at 12 months, highlighting that program quality and responsiveness may matter more than categorical segregation.
Subgroup data suggest that women-only formats may benefit women with high psychiatric severity or higher exposure to interpersonal trauma.
Pilot randomized work indicates that women with high psychiatric symptom severity may show greater reductions in substance use when assigned to women-focused group therapy compared to mixed-gender group counseling, with effect sizes in the medium to large range despite small samples.
Provider perspectives emphasize moving beyond isolated women-only services to integrate gender expertise across the whole treatment system. This includes outpatient and residential options that accommodate mothers with children, crisis and detox customized for women, accessible online support, and services that address stigma.
This systems lens suggests that even within mixed-gender settings, integrating gender-responsive features can expand access, reduce dropout, and improve downstream outcomes.
Social and Environmental Context Shapes Recovery
Across genders, not having a drug-using spouse or partner during follow-up is associated with abstinence at 12 months. For men, spousal drug use was a baseline predictor of poorer abstinence.
This underscores a crucial implication for gender-specific recovery plans: assessment and active management of partner risk exposure, such as couples-based interventions where safe, safety planning in contexts of intimate partner violence, or sober living arrangements when appropriate.
For women, interpersonal safety and trauma histories further complicate relational dynamics, necessitating integrated supports. Women’s outcomes and retention are often influenced by parenting status and child welfare involvement.
Programs allowing mothers to live with children or providing childcare can reduce barriers to attendance and completion. Conversely, stress of legal involvement can impede stability unless addressed with targeted supports.
These programmatic features may not directly alter 12-month abstinence in all cohorts but are key modulators of retention, thereby indirectly influencing long-term outcomes.
Recent machine-learning work highlights that linking clients to a primary care provider and facilitating access to SNAP increases the likelihood of attending self-help during treatment and setting goals, which are proximal behaviors that drive retention and completion.
Gender-responsive case management should formalize such linkages to reduce instability around food, health, and housing that disrupts treatment continuity, an especially salient issue for women with caregiving responsibilities.
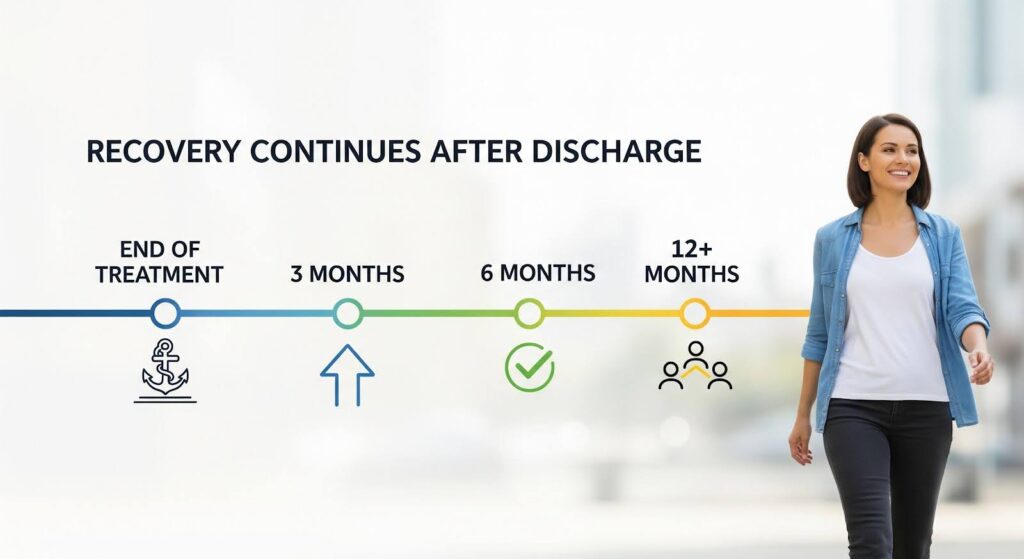
Early Gains Consolidate After Discharge
Multiple studies report early reductions in substance use at end-of-treatment and continued improvement by three months, suggesting that discharge planning should not only aim to prevent relapse but to actively consolidate gains.
The women veterans’ randomized trial observed additional reductions in drug severity between end-of-treatment and three-month follow-up, indicating that some gains consolidate only after discharge, particularly when recovery networks and self-efficacy grow.
This implies that discharge planning should be conceptualized as an activation point for continued care, not an endpoint. Structured aftercare that integrates mutual-help and professional supports for at least 12 months can help sustain early improvements.
Evidence indicates that abstinence at six months predicts abstinence at five years in alcohol and drug treatment populations. Among those abstinent at six months, predictors of five-year abstinence included older age, being female, 12-step attendance, and recovery-oriented social networks.
Why Does it Matter for Long-Term Success?
The best predictors of 12 to 24 month recovery success in gender-specific rehab are not the gender-segregated format per se, but the interaction of retention, sustained recovery network participation, and the removal of gendered barriers that impede engagement.
Practically, this means building programs that maximize retention and post-discharge recovery engagement rather than relying on women-only designation to carry the effect.
Embedding gender-responsive supports such as childcare, trauma-informed care, safe housing pathways, partner risk management, and flexible scheduling improves the proximal drivers like meeting attendance and goal setting that predict retention and long-term outcomes.
Systematically addressing partner or spousal drug use exposure and social instability is essential, as these undermine long-term abstinence irrespective of program format.
Programs should prioritize retention-first designs, activate mutual-help participation during treatment, set explicit recovery goals, link to primary care and social supports that stabilize life context, and customize supports for subgroups such as women with high psychiatric severity or mothers with children.
Implemented in concert, these elements convert early gains into durable recovery trajectories over 12 to 24 months.
If you or someone you care about is navigating recovery and needs support that addresses the whole person, reach out to our team to learn how our therapeutic community can help build a foundation for lasting change.
