
Leaving treatment early is one of the biggest obstacles to lasting recovery. Many people enter residential programs with hope but struggle to stay through the full episode of care.
Research shows that spiritual engagement during treatment can help people stick with their recovery plan and complete the program. When residential programs offer on-site 12-step meetings, sponsor connections, and spiritually oriented aftercare, patients build social support and a sense of purpose that make it easier to stay engaged.
This article explains how spiritual practices improve retention in residential treatment and what makes these approaches effective.
What Spiritual Engagement Means in Residential Treatment?
Spiritual engagement in substance use disorder care typically involves participation in 12-step activities like Alcoholics Anonymous or Narcotics Anonymous.
These include attending meetings, working with a sponsor, completing step work, reading recovery literature, and taking on service roles. In residential settings, programs often bring meetings on-site and use 12-step facilitation to help patients connect with mutual-help communities during their stay.
The goal is not to impose beliefs but to offer structured opportunities for people who find meaning and support in spiritual practices. When programs embed these activities into daily routines, they lower barriers to participation and help patients build habits that support long-term recovery.
How Spiritual Practices Support Treatment Retention?
Several mechanisms explain why spiritual engagement can improve retention and completion rates in residential care.
Social Support and Peer Accountability
Regular group participation creates bonds that increase treatment engagement. When patients attend on-site meetings and connect with sponsors, they gain peer accountability and mutual aid. These relationships can reduce dropout tendencies by providing encouragement during difficult moments and reinforcing commitment to the treatment plan.
Identity Transformation and Meaning-Making
12-step philosophies help people shift from seeing themselves as “addicts” to viewing themselves as “people in recovery.” This identity change is sustained by spiritual practices that reinforce perseverance during treatment challenges. Journaling, goal setting, and reflection activities give patients a sense of purpose that extends beyond symptom management.
Structured Routines and Behavioral Activation
Regular attendance at meetings and active roles in mutual-help groups increase behavioral activation and reduce idle time. This structure indirectly supports adherence to residential routines by filling the day with meaningful activities and reducing opportunities for rumination or disengagement.
Evidence Linking Spiritual Engagement to Retention
Direct causal evidence that spiritual engagement alone increases residential retention is limited. Most rigorous studies prioritize substance use outcomes like abstinence and psychosocial improvement rather than length of stay or completion rates.
However, converging signals from related research support a plausible, positive association when spiritual engagement is actively facilitated on-site and integrated with evidence-based care.
On-Site Meetings and Engagement Intensity
Programs offering on-site 12-step meetings during treatment report increased subsequent meeting attendance and engagement, as well as longer post-treatment abstinence.
Early, frequent, and active involvement in 12-step activities predicts better outcomes more strongly than attendance alone. Meeting frequency of three or more per week, combined with active roles like sponsorship and service, correlates with sustained abstinence after discharge.
These findings suggest that deeper spiritual engagement relates to behavioral persistence and adherence, features that plausibly extend to in-program retention and eventual treatment completion.
Integration with Medication for Opioid Use Disorder
A prospective study of a 12-step-based residential and day treatment center that integrated buprenorphine-naloxone and naltrexone found that nearly all patients completed residential care.
Among those who elected to use medication, compliance at one and six months was associated with significantly higher abstinence. This demonstrates that spiritual programming can coexist with pharmacotherapy, though causality for retention cannot be isolated from the combined model.
National data from the Treatment Episode Data Set show that medication for opioid use disorder is associated with a 40 percent increase in treatment completion and a 34 percent increase in retention in short-term residential programs.
In long-term programs, the association is weaker or neutral. These findings suggest that programs combining structured spiritual engagement with medication access are likely to achieve superior retention and completion in short-term settings.
Transitional Care Strategies That Reinforce Spiritual Engagement
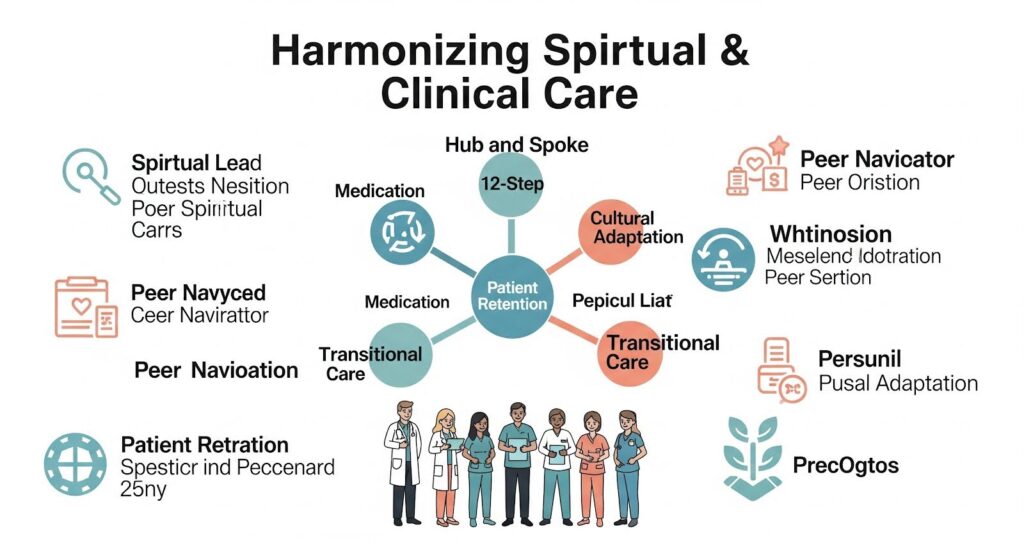
Spiritual engagement during residential treatment is most effective when it connects to ongoing support after discharge. Transitional care strategies like bridge clinics, peer navigation, and telemedicine improve post-discharge linkage and retention by ensuring patients have clear next steps and immediate access to care.
A scoping review of 52 studies on hospital-initiated medication for opioid use disorder and discharge linkage found that transitional strategies increased outpatient linkage, reduced readmissions, and improved retention.
These strategies are conceptually applicable to residential discharge. Embedding peer recovery supports, ensuring rapid-access follow-up, and leveraging telehealth can complement spiritual engagement by converting in-program motivation into continuity of care.
Structured discharge planning that includes ongoing 12-step engagement, sponsor contact, and contingency strategies helps patients sustain the habits they built during residential care. This reduces anxiety about what comes next and decreases the risk of early exit.
Cultural Adaptation and Spiritual Engagement
For populations whose spiritual traditions are integral to identity and community life, culturally congruent spiritual engagement may be particularly effective in sustaining residential participation and completion.
A systematic review of culturally tailored substance use interventions for Indigenous populations documents programs that center culture through talking circles, ceremonies, and mutual-help practices like culturally adapted AA and Wellbriety.
These adaptations appear to enhance accessibility and engagement. Several studies reported improved participation and retention-related outcomes, though methodological limitations temper definitive conclusions. The likely pathway is increased trust, reduced cultural dissonance, and enhanced perceived relevance of the program.
A broader meta-analysis of culturally adapted substance use disorder interventions suggests these approaches can improve initiation and retention among marginalized populations, though high-quality studies remain limited and adaptation approaches vary.
Application to spiritual engagement includes tailoring 12-step content, language, and rituals to resonate with cultural values.

Comparing Spiritual Engagement with Other Evidence-Based Practices
To understand the role of spiritual engagement, it helps to compare it with other interventions that have strong evidence for improving retention and abstinence.
| Intervention | Primary Mechanisms | Evidence for Retention and Abstinence |
| 12-step facilitation and on-site meetings | Mutual-help linkage, recovery identity, peer support | Indirect evidence; improves engagement and post-discharge abstinence |
| Medication for opioid use disorder | Reduces cravings and withdrawal | 40% increase in completion and 34% increase in retention in short-term residential programs |
| Contingency management | Contingent reinforcement for attendance and abstinence | Improves abstinence and retention in outpatient settings; combined with community reinforcement approach, increases end-of-treatment abstinence |
| Community Reinforcement and Family Training | Behavioral training for family members to engage unmotivated users | Higher engagement into treatment than Al-Anon or Nar-Anon facilitation |
The strongest causal signals for improving completion and retention in short-term residential care come from medication for opioid use disorder. Spiritual engagement is consistently associated with improved post-discharge outcomes and stronger engagement during and after treatment.
When facilitated on-site, it likely enhances treatment adherence and supports completion, though causal retention evidence is weaker than for medication.
Practical Recommendations for Residential Programs
Residential programs can integrate spiritual engagement in ways that support retention and completion while respecting patient preferences and maintaining evidence-based care.
Embed Spiritual Engagement as an Operational Practice
- Offer on-site 12-step meetings multiple times per week.
- Implement 12-step facilitation elements like structured orientation, linkage to volunteers and sponsors, and problem-solving barriers to participation.
- Track engagement metrics such as attendance frequency and active roles as part of routine outcomes monitoring.
Integrate Medication and Align It with Spiritual Programming
- Ensure equitable access to buprenorphine and naltrexone.
- Educate staff and peers to harmonize pharmacotherapy with 12-step participation.
- Monitor adherence and address relapse risks with tailored supports beyond medication, particularly for those who relapse post-discharge.
Strengthen Transitional Care
- Pre-schedule bridge appointments for same-day or next-day access and telemedicine follow-ups.
- Embed peer navigators to conduct warm handoffs to outpatient care and mutual-help communities.
- Create structured discharge plans that include ongoing 12-step engagement, sponsor contact, and contingency strategies.
Culturally Adapt Spiritual Engagement
- For Indigenous and other marginalized groups, collaborate with community leaders to adapt 12-step content and integrate culturally meaningful spiritual practices.
- Invest in bilingual and culturally competent staffing where indicated.
Why Does it Matter?
Retention in residential treatment is a critical determinant of long-term recovery outcomes. When people complete their planned episode of care, they are more likely to sustain abstinence, rebuild relationships, and avoid relapse. Spiritual engagement offers a pathway to deeper connection, meaning, and social support that can help people stay engaged during the challenging early weeks of treatment.
The optimal approach for enhancing retention and completion in short-term residential settings is an integrated model that combines spiritual engagement through on-site 12-step facilitation, medication for opioid use disorder, and structured transitional care. In long-term programs, the association between medication and completion is weaker or negative, so spiritual engagement may still offer engagement and psychosocial benefits, but program-specific design and measurement are crucial.
Cultural adaptation of spiritual content further enhances engagement and likely retention among marginalized groups by increasing program relevance and trust. The literature supports the importance of deep adaptation beyond translation, including community-led design and incorporation of culturally grounded spiritual practices.
If you or someone you care about is considering residential treatment, look for programs that offer a range of evidence-based services and respect individual preferences around spiritual practices. Recovery is deeply personal, and the right program will meet you where you are.
Ready to explore your options? Learn more about addiction counseling that integrates spiritual support with proven clinical care.
